By Attila Hertelendy, Craig Fugate and Gregory R. Ciottone
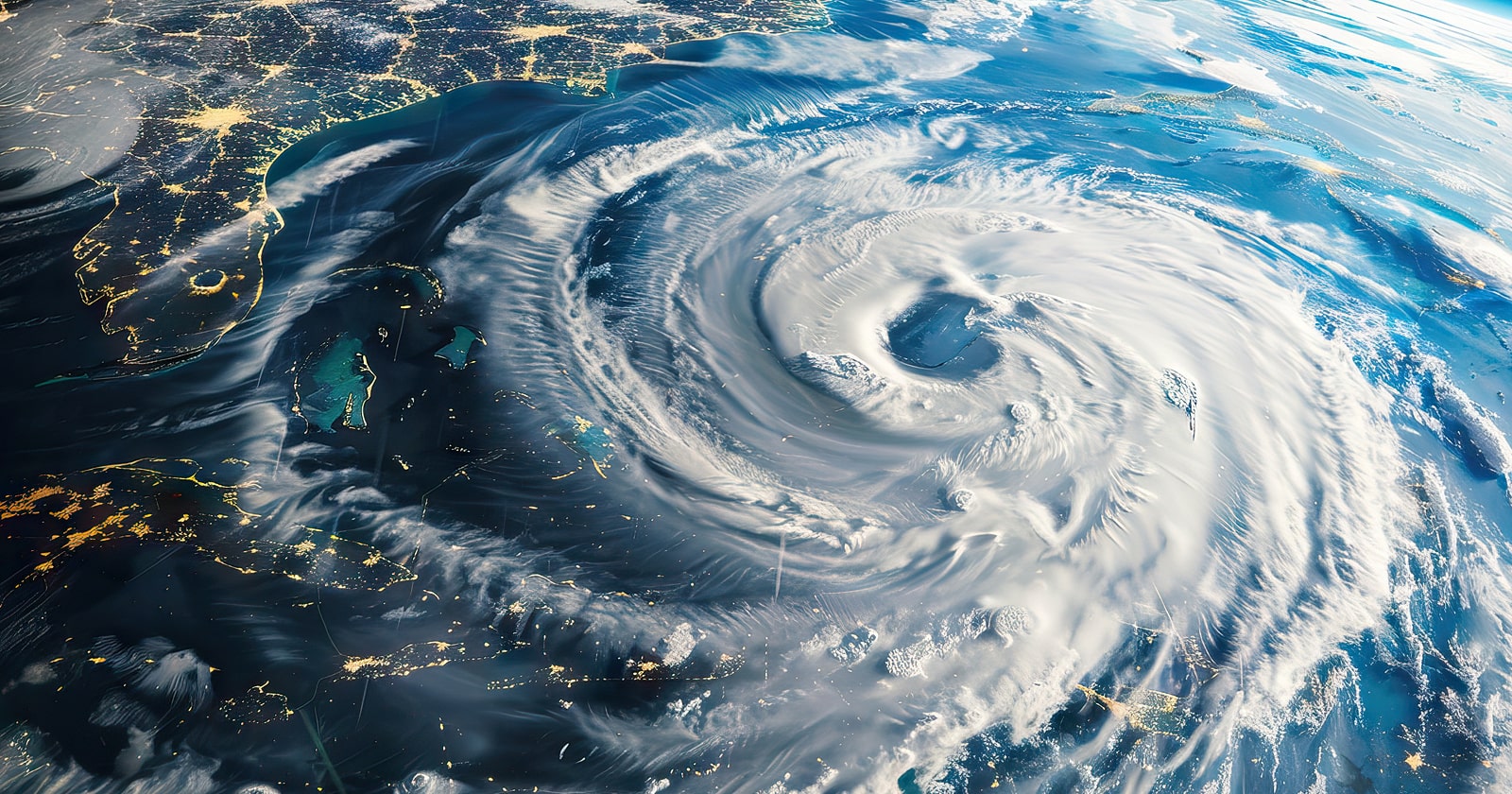
Cyclonic storms are natural disasters that can be predicted to occur seasonally in certain parts of the world. Along with Caribbean islands, it is likely that the eastern and southern coastlines of the United States will experience the impact of at least one significant storm each year during hurricane season. The 2024 Atlantic Hurricane season begins June 1 through November 30. Forecasters at the National Oceanic Atmospheric Administration (NOAA) predict an 85% chance of an above normal hurricane season in the Atlantic Basin.1 The agency predicts 17–24 named storms the highest in any preseason forecast on record. Of these 4–7 are expected to be major hurricanes category (3,4, or 5 with winds of 111 mph or greater). 1 Hurricane Beryl is the first of the 2024 Atlantic season, which was unusually early in the year. It strengthened to a Category 5 storm that made landfall in Jamaica, St. Vincent and the Grenadines, Barbados and Mexico, killing at least 11 people throughout the Caribbean.2,3 Human caused climate change is resulting in global warming of oceans and in the Atlantic basin, melting of ice on land, glaciers in northern Canada and Greenland are leading to sea level rise which significantly impacts the risk of storm surge.
Hurricane Ian in 2022 devastated western Florida becoming the seventh deadliest hurricane in US history with 66 total direct deaths attributed to the storm of which 41 were a result of storm surge. The leading causes of death were blunt trauma and drowning due to storm surge and flooding, particularly in Lee County, Florida. Freshwater flooding caused additional fatalities in central and eastern Florida.
Several lessons were learned from hurricane Ian that are instructive for healthcare systems to consider to adequately prepare and respond to future hurricanes.
- Misplaced focus on the National Hurricane Centers (NHC) forecast cone: The public concentrated on the NHC Forecast Cone, which only indicates the probable path of the storm's center, rather than understanding the broader impact areas. Large storms like Hurricane Ian have effects that extend well beyond the cone and may not follow the predicted forecast cone.
- Delayed Evacuation Orders: Local officials delayed issuing evacuation orders, which reduced the time available for residents to safely evacuate from high-risk areas. This delay contributed to higher fatalities during the storm.
- Underestimating Water Risks: People tend to underestimate the dangers of water (storm surge and flooding) compared to wind during hurricanes. This leads to inadequate preparation and response to water-related threats.
A hospital's ability to operate when resources are strained, and patient surge is occurring is an important component of hospital resilience. This expertise in crisis healthcare is particularly important now, given the substantially higher number of impactful storms predicted for the 2024 hurricane season, and the state of emergency department overcrowding we are now seeing in hospitals across the country that limits surge capacity.
When a natural disaster like a hurricane strikes, the effectiveness of the healthcare response is determined by how well-prepared systems are and their level of readiness, which can be enhanced by taking proactive steps to build local healthcare capability and capacity.
These steps include ensuring hospital disaster plans are reviewed and updated to include: clear communication protocols, defined roles and responsibilities (especially of off duty staff), facility access and transportations plans, shelter and accommodations, family support plans for staff, psychological support, compensation and incentive policies, mutual aid agreements, and evaluation and improvement through after-action reviews.
Increasingly, healthcare systems are being impacted by complex emergencies. This occurs where multiple crisis compound and can occur in parallel such as a natural disaster, public health emergency (pandemic or epidemic) cyberattacks, conflict, civil war or political strife.
Healthcare systems should consider outside the box thinking when it comes to disaster preparedness and response. Leaders faced with multiple crisis occurring potentially at the same time will need to question existing preparedness and response paradigms. This requires a shift in thinking beyond minimum adherence to joint commission requirements for emergency preparedness. The goal of health systems resiliency is to maintain an ability to provide non-interrupted patient care services during a crisis. This will increasingly require the need for not only qualified hospital emergency managers in all hospitals, but also clinicians who are trained as disaster medicine specialists.
Healthcare leaders should be thinking about implementing innovative ways to keep staff trained and ready by providing high fidelity simulations, and realistic live exercises. An example pertinent to hurricane preparedness would be to simulate operating a hospital for 96 h on diesel generators while at the same time coordinating a response to both a hurricane and cyberattack. The challenge with this scenario is fuel for diesel generators. In some states, hospitals are required to maintain no less than 64 h runtime. Most recommendations state 96 h, with higher fuel storage in rural and remote locations. According to Craig Fugate, former FEMA administrator, in 2005 after Hurricane Wilma, diesel fuel for generators became a critical issue as most officials had not planned on Port Everglades losing power and the subsequent port closure due to Wilma (Fugate, C., FEMA, personal communication). Also, with all the generators in operation, diesel consumption was exceeding supply of delivery trucks and available fuel.
By implementing a proactive hospital emergency management program that involves the mitigation and preparedness steps required for an efficient and effective response, hospitals will be taking the necessary steps to maximize their readiness for this upcoming hurricane season.
About the Authors:
Attila Hertelendy is associate teaching professor of information systems and business analytics at FIU Business.
Hertelendy co-authored the article with Craig Fugate of Beth Israel Deaconess Medical Center and Gregory R. Ciottone of Harvard Medical School.